
Cardiorenal and Metabolic Diseases Research Center
The Cardiorenal and Metabolic Diseases Research Center (CMDRC) at the University of Mississippi Medical Center has been supported for over 10 years by an award from the National Institute of General Medical Sciences (NIGMS). The NIGMS is a part of the National Institutes of Health (NIH) that supports thematic, multidisciplinary Centers of Biomedical Research Excellence (COBRE) across the country through its Institutional Development Award (IDeA) program.
Cardiovascular, renal and metabolic diseases are inextricably linked and are the leading causes of mortality and morbidity in the United States, especially in Mississippi which has the highest prevalence in the nation of these diseases. These disorders usually cluster together and are highly interdependent. For example, obesity and associated metabolic disorders, such as diabetes, are major causes of cardiovascular and renal disease.
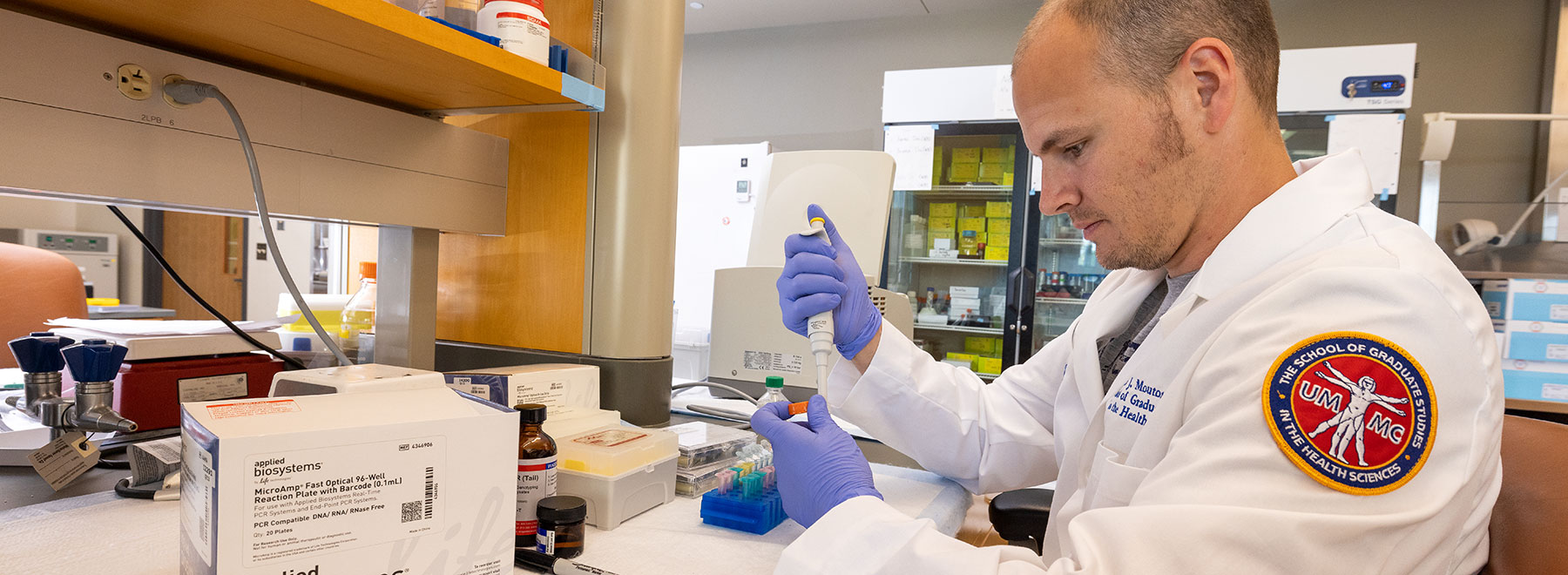
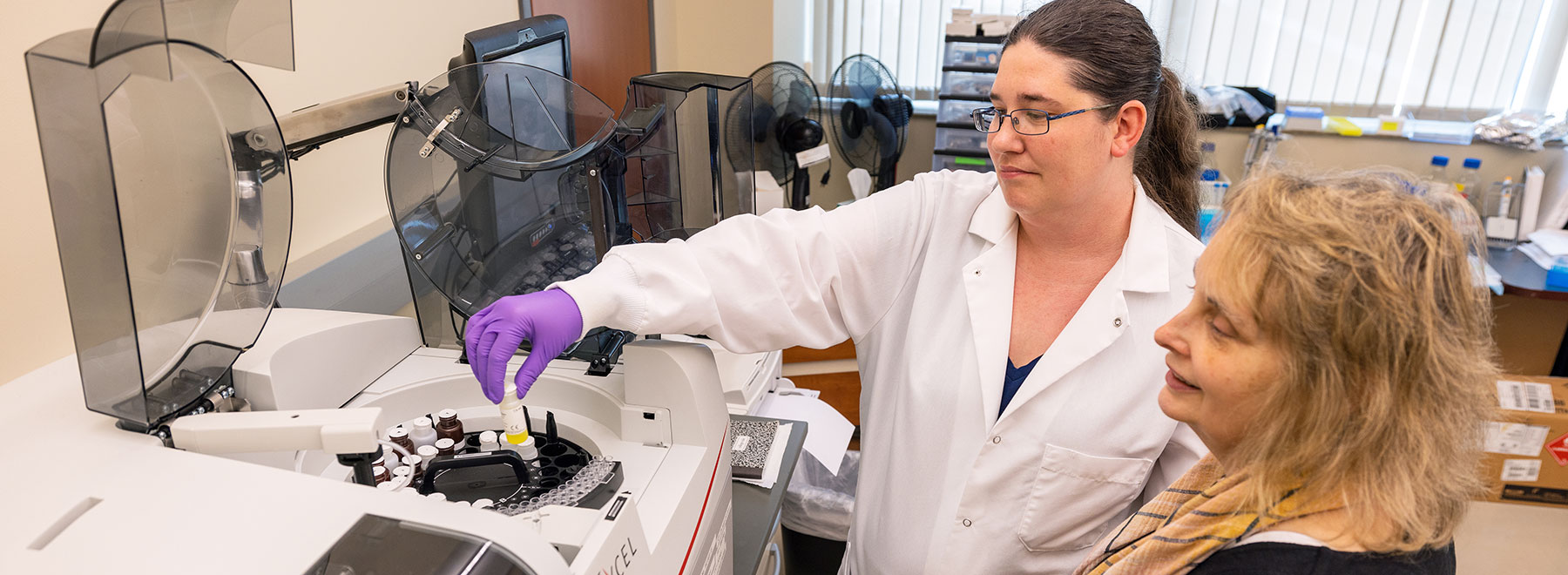
A major objective in developing the Cardiorenal and Metabolic Diseases Research Center is to provide infrastructure for a varied, multidisciplinary group of basic, clinical and population scientists working on the common synergistic theme of obesity, cardiorenal and metabolic diseases and to facilitate their collaborations.
Kudos